Abstract
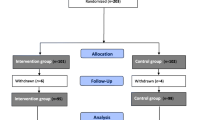
This study aimed to determine effects of a Multidisciplinary Intensive Education Programme (MIEP) based on the empowerment approach for diabetic patients with prolonged self-management difficulties. In 89 participants, glycaemic control (HbA1c), health related quality of life (HR-QoL) and indicators of empowerment were measured before MIEP (10 days in 10 weeks, follow-up after 6 and 12 weeks) and at 12 weeks follow-up. The participants were compared with 231 average outpatients who were measured once. Overall, participants improved their glycaemic control, mental health, satisfaction with treatment and became more empowered. Subgroup analyses revealed that especially patients with poor baseline control improved their HbA1c. At baseline, participants with poor mental health scored worse on all other HR-QoL subscales too and were less empowered compared to the satisfactory mental health group. The poor mental health participants improved in most of these aspects. MIEP has beneficial effects in HbA1c, HR-QoL, and empowerment, especially in patients with poor status at baseline.
Similar content being viewed by others
References
American Diabetes Association (ADA) (2001). Standards of Medical Care for Patients With Diabetes Mellitus. Diabetes Care [On-line]. Available: http://www.journal.diabetes.org.
Anderson, R. M., Funnell, M. M., Barr, P. A., Dedrick, R. F., & Davis, W. K. (1991). Learning to empower patients. Results of professional education program for diabetes educators [published erratum appears in Diabetes Care 1991 Oct;14(10):933]. Diabetes Care, 14, 584–590.
Anderson, R. M., Funnell, M. M., Butler, P. M., Arnold, M. S., Fitzgerald, J. T., & Feste, C. C. (1997). Patient empowerment. Results of a randomized controlled trial. Diabetes Care, 18, 943–949.
Anderson, R. M., Funnell, M. M., Carlson, A., Saleh-Statin, N., Cradock, S., & Skinner, T. C. (2000). Facilitating self-care through empowerment. In F. J. Snoek & T. C. Skinner (Eds.), Psychology in diabetes care (1st ed., pp. 69–98). Chichester: Wiley.
Berger, M., & Muhlhauser, I. (1999). Diabetes care and patient-oriented outcomes. JAMA, 281, 1676–1678.
Bott, U., Bott, S., Hemmann, D., & Berger, M. (2000). Evaluation of a holistic treatment and teaching programme for patients with type 1 diabetes who failed to achieve their therapeutic goals under intensified insulin therapy. Diabetic Medicine, 17, 635–643.
Campbell, D. T., & Kenny, D. A. (1999). A primer on regression artifacts (1st ed.). New York: The Guilford Press.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159.
Colagiuri, R., Colagiuri, S., & Naidu, V. (1995). Can patients set their own educational priorities? Diabetes Research and Clinical Practice, 30, 131–136.
Dalewitz, J., Khan, N., & Hershey, C. O. (2000). Barriers to control of blood glucose in diabetes mellitus. American Journal of Medical Quality, 15, 16–25.
Diabetes Control and Complications Trial Research Group (1988). Reliability and validity of a diabetes quality-of-life measure for the diabetes control and complications trial (DCCT). The DCCT Research Group. Diabetes Care, 11, 725–732.
Diabetes Control and Complications Trial Research Group (1993). The effects of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine, 329, 977–986.
Diabetes Control and Complications Trial Research Group (DCCT) (1996). Influence of intensive diabetes treatment on quality-of-life outcomes in the diabetes control and complications trial [see comments]. Diabetes Care, 19, 195–203.
Dunn, S. M., Bryson, J. M., Hoskins, P. L., Alford, J. B., Handelsman, D. J., & Turtle, J. R. (1984). Development of the diabetes knowledge (DKN) scales: Forms DKNA, DKNB, and DKNC. Diabetes Care, 7, 36–41.
European Diabetes Policy Group 1998–1999 (1999). A Desktop Guide to Type 2 Diabetes Mellitus. International Diabetes Federation European Region [On-line]. Available: http://www.staff.newcastle.ac.uk/philip.home/t2dg1999.htm.
Feste, C. (1992). A practical look at patient empowerment. Diabetes Care, 15, 922–925.
Fosbury, J. A., Bosley, C. M., Ryle, A., Sonksen, P. H., & Judd, S. L. (1997). A trial of cognitive analytic therapy in poorly controlled type I patients. Diabetes Care, 20, 959–964.
Funnell, M. M., Anderson, R. M., Arnold, M. S., Barr, P. A., Donnelly, M., Johnson, P. D., et al. (1991). Empowerment: An idea whose time has come in diabetes education. Diabetes Educator, 17, 37–41.
Glasgow, R. E. (1999). Outcomes of and for diabetes education research. Diabetes Educator, 25, 74–88.
Glasgow, R. E., Eakin, E. G., & Toobert, D. J. (1996). How generalizable are the results of diabetes self-management research? The impact of participation and attrition. Diabetes Educator, 22, 573–2,584.
Glasgow, R. E., & Osteen, V. L. (1992). Evaluating diabetes education. Are we measuring the most important outcomes? Diabetes Care, 15, 1423–1432.
Halfens, R. (1985). De beheersingsorientatie in Relatie tot Ziekte-en Gezondheidsgedrag. Thesis.
Hanestad, B. R., & Albrektsen, G. (1991). Quality of life, perceived difficulties in adherence to a diabetes regimen, and blood glucose control. Diabetic Medicine, 8, 759–764.
Jacobson, A. M. (1996). The psychological care of patients with insulin-dependent diabetes mellitus. New England Journal of Medicine, 334, 1249–1253.
Jacobson, A. M., & Diabetes Control and Complications Trial Research Group (1994). The diabetes quality of life measure. In C. Bradley (Ed.), Handbook of psychology and diabetes (pp. 65–87). Amsterdam: Harwood Academic Publishers.
Keers, J. C., Blaauwwiekel, E. E., Hania, M., & Boujma, J. (2004). Diabetes rehabilitation: Development and first results of a Multidisciplinary Intensive Education Program for patients with prolonged self-management difficulties. Patient Education and Counseling, 52, 151–157.
Kempen, G. I. J. M., Miedema, I., Van den Bos, G. A. M., & Ormel, J. (1998). Relationship of domain-specific measures of health to perceived overall health among older subjects. Journal of Clinical Epidemiology, 51, 11–18.
Kempen, G. I. J. M., Ormel, J., Brilman, E. I., & Relyveld, J. (1997). Adaptive responses among Dutch elderly: The impact of eight chronic medical conditions on health-related quality of life. American Journal of Public Health, 87, 38–44.
Lloyd, C. E., Dyer, P. H., Lancashire, R. J., Harris, T., Daniels, J. E., & Barnett, A. H. (1999). Association between stress and glycemic control in adults with type 1 (insulin-dependent) diabetes. Diabetes Care, 22, 1278–1283.
Macrodimitris, S. D., & Endler, N. S. (2001). Coping, control, and adjustment in type 2 diabetes. Health Psychology, 20, 208–216.
Mulcahy, K., Peeples, M., Tomky, D., & Weaver, T. (2000). National Diabetes Education Outcomes System: Application to practice. Diabetes Educator, 26, 957–964.
Norris, S. L., Engelgau, M. M., & Narayan, K. M. (2001). Effectiveness of self-management training in type 2 diabetes; a systematic review of randomized controlled trials. Diabetes Care, 24, 561–587.
Peyrot, M. (1999). Behavior change in diabetes education. Diabetes Educator, 25, 62–73.
Peyrot, M., & Rubin, R. R. (1994). Modeling the effect of diabetes education on glycemic control. Diabetes Educator, 20, 143–148.
Rubin, R. R., & Peyrot, M. (1992). Psychosocial problems and interventions in diabetes. A review of the literature. Diabetes Care, 15, 1640–1657.
Schwartz, L. S., Coulson, L. R., Toovy, D., Lyons, J. S., & Flaherty, J. A. (1991). A biopsychosocial treatment approach to the management of diabetes mellitus. General Hospital Psychiatry, 13, 19–26.
Snoek, F. J., Van der Ven, N. C. W., & Lubach, C. (1999). Cognitive behavioral group training for poorly controlled type 1 diabetes patients: A psychoeducational approach. Diabetes Spectrum, 12, 147–152.
Surgenor, L. J., Horn, J., Hudson, S. M., Lunt, H., & Tennent, J. (2000). Metabolic control and psychological sense of control in women with diabetes mellitus. Alternative considerations of the relationship. Journal of Psychosomatic Research, 49, 267–273.
Talbot, F., Nouwen, A., Gingras, J., Belanger, A., & Audet, J. (1999). Relations of diabetes intrusiveness and personal control to symptoms of depression among adults with diabetes. Health Psychology, 18, 537–542.
Tillotson, L. M., & Smith, M. S. (1996). Locus of control, social support, and adherence to the diabetes regimen. Diabetes Educator, 22, 133–139.
UKPDS (1998). Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group [see comments]. Lancet, 352, 837–853.
Van der Zee, K., Sanderman, R., Heyink, J. W., & De Haes, H. (1996). Psychometric qualities of the RAND 36-item Health Survey 1.0: A multidimensional measure of general health status. International Journal of Behavioural Medicine, 3, 104–122.
Ven, N. C. W. V. d., Chatrou, M., & Snoek, F. J. (2000). Cognitive-behavioural group training. In F. J. Snoek & T. C. Skinner (Eds.), Psychology in diabetes care (1 ed., pp. 207–234). Chichester: Wiley.
Wallston, K., Stein, M., & Smith, C. (1994). Form C of the MHLC scales: A condition-specific measure of locus of control. Journal of Personality Assessment, 63, 534–553.
Wallston, K. A., Wallston, B. S., & DeVellis, R. (1978). Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Education Monographs, 6, 160–170.
Ware, J. E., & Sherbourne, C. D. (1992). The MOS 36-item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Medical Care, 30, 473–483.
Watkins, K. W., Connell, C. M., Fitzgerald, J. T., Klem, L., Hickey, T., & Ingersoll-Dayton, B. (2000). Effect of adults’ self-regulation of diabetes on quality-of-life outcomes. Diabetes Care, 23, 1511–1515.
Welch, G. (1994). Diabetes coping measure. In C. Bradley (Ed.), Handbook of psychology and diabetes: A guide to psychological measurement in diabetes research and practice (pp. 400). London: Harwood Academic Publishers.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keers, J.C., Links, T.P., Bouma, J. et al. Diabetes Rehabilitation: Effects of a Multidisciplinary Intensive Education Programme for Diabetic Patients with Prolonged Self-Management Difficulties. J Clin Psychol Med Settings 12, 117–126 (2005). https://doi.org/10.1007/s10880-005-3272-y
Issue Date:
DOI: https://doi.org/10.1007/s10880-005-3272-y