Abstract
Neurogenic bladder is a heterogeneous entity that may result from a variety of conditions affecting the central or peripheral nervous systems. Regardless of etiology, the overall goals of management are primarily twofold. As a neurogenic bladder may affect the ability to store urine safely and to empty the bladder efficiently, early management is focused on optimization of bladder storage function to prevent irreversible injury to either the upper or lower urinary tracts. In older children, this goal is added to the challenge of maximizing quality of life through achievement of urinary continence and independence in bladder management that continues into the transition to adulthood.
In this review, we seek to bring the reader up-to-date regarding management of the pediatric neurogenic bladder with a focus on literature published in the past year. We discuss key contributions related to fetal intervention for myelomeningocele, monitoring and medical management of the neurogenic bladder and prediction of postoperative outcomes. Put together, these studies highlight the continued need for further research to improve evidence-based medical and surgical decision-making strategies for children affected by neurogenic bladder.
Similar content being viewed by others
Introduction
The normal lower urinary tract allows for both coordinated low-pressure filling and periodic voluntary bladder emptying. Given the complexity of its neural control, central or peripheral nervous system lesions that affect the parasympathetic, sympathetic or somatic systems may have varied effects on the lower urinary tract. Thus, a neurogenic bladder in children may occur secondary to central nervous system (CNS) lesions such as cerebral palsy, spinal dysraphisms and spinal cord injury or secondary to pelvic pathology such as tumors and anorectal malformations.
The goals in management of the neurogenic bladder are primarily twofold. As a neurogenic bladder may affect the ability to store urine safely and to empty the bladder efficiently, early management is focused on optimization of bladder function to prevent irreversible morphological and functional injury to either the upper or lower urinary tracts. In older children, this goal is added to the challenge of maximizing quality of life through achievement of urinary continence and independence in bladder management.
In this review, we seek to bring the reader up-to-date regarding management of the pediatric neurogenic bladder with a focus on literature published in the past year. We will discuss key contributions related to fetal intervention for myelomeningocele, monitoring and medical management of the neurogenic bladder and prediction of postoperative outcomes. Put together, these studies highlight the continued need for further research to improve evidence-based medical and surgical decision-making strategies for children affected by neurogenic bladder.
Myelomeningocele: Fetal Surgery and Urinary Tract Outcomes
Although an initial decline in incidence of myelodysplasia was observed following widespread folate supplementation, the incidence of 3.7 per 10,000 live births in the United States [1] has stabilized during the past decade [2]. Given its substantial long-term morbidity and potential to impact neurologic development, prenatal closure of the open myelomeningocele defect has been initiated in specialized centers. While fetal closure has been associated with improvement in hydrocephalus and motor function, early reports of its effect on the urinary tract have been less promising [3–5].
The Management of Myelomeningocele Study (MOMS) was a randomized prospective clinical trial evaluating prenatal versus neonatal closure of open myelomeningocele. Early trial outcomes included decreased CSF shunt placement rates and improved mental development and motor function measures at age 30 months following in utero closure [6]. However, a subsequent evaluation of urologic outcomes found no difference in the rates of children meeting criteria for initiation of clean intermittent catheterization (CIC) by 30 months (38 versus 51 % of the prenatal and postnatal surgery groups respectively; RR 0.74, 95 % CI 0.48–1.12). Secondary effects included less trabeculation in the prenatal surgery cohort and, after adjustment for gender and lesion level, a decrease in the presence of bladder diverticulae and open bladder neck during filling [7•].
In the past year, two additional institutional series evaluating urinary tract outcomes following prenatal myelomeningocele closure were published. In the first series, only two of 48 infants at a mean age of 5.4 months had a normal bladder on urodynamics while findings that may place the upper tracts at increased risk (end fill or detrusor leak point pressure (EFP or DLPP) of >40 cm/H20) were present in 56 %. Furthermore, upper tract changes were present early with hydronephrosis or vesicoureteral reflux (VUR) observed in 26 % [8]. In a second series of 58 children followed up to 5 years after prenatal closure, only 19 % were successfully toilet-trained [9]. Additional long-term assessment will continue to provide information regarding the effects of in utero closure on the urinary tract. In the interim, these findings emphasize the importance of educating parents that ongoing urologic assessment and management are essential for children post prenatal myelomeningocele closure as they remain at significant risk for the development of a neurogenic bladder.
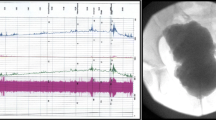
Radiologic and Urodynamic Assessment of the Neurogenic Bladder
The current options available to evaluate the neurogenic bladder and upper tracts include ultrasonography (US), fluoroscopy, nuclear medicine studies or urodynamic testing. As was discussed in a recent review regarding the urologic management of spina bifida [10••], there is a current debate regarding the optimal role and timing of these studies fueled by a desire to prevent excessive invasive testing and radiation exposure. This debate is reflected in recent literature that has evaluated the diagnostic and prognostic value of each test including the use of nuclear medicine studies versus US in evaluation of the upper urinary tract, non-invasive methods of bladder wall assessment and urodynamics in children undergoing tethered cord release (TCR).
Evaluation of Renal Scarring: DMSA Versus US
Regardless of management strategy, the goal to detect early upper tract changes that may precede deterioration is key to long-term prevention of renal failure. Prior series of children with myelodysplasia have demonstrated rates of renal scarring or functional loss of 10-32 % on DMSA nuclear medicine scans [11–14]. As a follow-up study, 122 adults with spina bifida were evaluated with both DMSA and US modalities to obtain a baseline assessment of renal scarring. A significant difference in renal scar detection was observed between US (10 %) and DMSA scans (46 %). Additionally, hypertension was only correlated with the presence of scarring on DMSA in this adult population [15•]. Recent literature evaluating the optimal imaging strategy following a febrile UTI in children likewise demonstrated that even the most optimized current model based on US findings has a low predictive value for either renal parenchymal anomalies or the presence of VUR [16]. Although the majority of these studies evaluated children with non-neurogenic bladders, [17] the lack of sensitivity of US for either VUR or renal scarring is of particular interest in neurogenic bladder given the need to prevent irreversible renal damage and the association of VUR with renal cortical loss in these children [11–14]. These findings require future evaluation but call into question the premise of an evaluation strategy that is reliant on US changes to precede further testing or intervention.
Non-invasive Monitoring of Lower Urinary Tract Function
There is ongoing need for improved methodologies to assess early alterations in the bladder wall that may portend development of poor compliance. Bladder wall hypertrophy with its associated morphologic changes may decrease bladder compliance through effects on smooth muscle, connective tissue, innervation and tissue hypoxia. The ultrasonographic assessment of the bladder wall as a clinically meaningful outcome requires the ability to reliably assess these changes early when an intervention may reverse or halt progression toward irreversible decompensation [18]. In the largest recent study evaluating the utility of bladder wall measurements by US in the neurogenic bladder, 272 adult patients with SCI were evaluated. Although no threshold wall thickness was predictive of urodynamic findings, BWT was significantly increased in individuals with neurogenic detrusor overactivity associated with detrusor sphincter dyssynergia (NDO/DSD) or impaired bladder compliance compared to those without DSD [19]. On the other hand, in the actively managed pediatric neurogenic bladder, this predictive capacity of BWT may be more elusive as demonstrated by multiple series with mixed results [20–22]. In particular, a recent study of 53 closely managed children with spina bifida found that BWT was not predictive of unfavorable urodynamic parameters even when measured at specified bladder volumes [23•]. To improve the predictive capability of non-invasive studies of the lower urinary tract, our center is currently evaluating alternative technologies including bladder elastography as a potential solution to the ongoing need for a non-invasive evaluation strategy for these children.
Predictive Urologic Changes in Tethered Cord Release
Urologic findings are often the first clinical sign in the up to one third of individuals who develop symptomatic tethering on long-term follow-up after postnatal myelomeningocele closure [24]. Two series were published in reference to secondary tethering and urologic outcomes of children in the past year. In a series of 23 children with secondary tethered cord, TCR significantly improved bladder compliance, DLPP and EFP. Urologic symptoms were improved in 62 % with all previously incontinent children reporting resolved or improved continence postoperatively [25]. These findings added to a growing body of literature evaluating clinical outcomes following primary TCR in occult spinal dysraphism. In a recent series from our institution, although asymptomatic children with cutaneous lesions had excellent continence rates post-TCR, no specific urodynamic parameters were associated with urologic outcomes [26]. Similarly, in a second series of 40 children although significant improvement in both continence and UTI rates were observed following secondary TCR, preoperative neurologic symptoms prompting TCR were not a predictor of urologic outcomes [27]. Taken together, an improvement in bladder dynamics or symptoms may be observed following either primary or secondary TCR. However, as the current ability to predict such changes is limited, urologic follow-up with a postoperative urodynamic evaluation may be warranted following these procedures.
Management of the Neurogenic Bladder
Prior to the widespread utilization of CIC for the management of neurogenic bladder, renal failure and urosepsis were common causes of long-term morbidity and mortality. Recent baseline data of 2172 participants in the National Spina Bifida Registry provides a window into current management. In the specialized centers participating, 74 % of participants with myelomeningocele and bladder impairment utilized CIC [28]. Fortunately, in this era of CIC incorporation into practice, long-term success has been achieved in preventing VUR and hydronephrosis, decreasing augmentation cystoplasty (AC) rates and reducing postoperative mortality secondary to renal failure [29–31]. The challenge remains, however, to identify children who would benefit from initiation of CIC and the optimal timing for each medical or surgical intervention currently available.
Medical Management
In a stepwise process of neurogenic bladder management, initial efforts at maintaining a compliant storage reservoir and treatment of urinary continence are focused on improved bladder drainage through catheterization and the addition of medications in an individualized manner. If the desired result is not achieved through anticholinergic therapy, another combination of medications, endoscopic management or neuromodulation may be utilized prior to surgical reconstructive procedures. Recent studies have focused on medical management alternatives and the efficacy of intravesical Botox for these children.
Anticholinergics and Pharmacologic Therapy
Anticholinergic therapy has been demonstrated to have both short- and long-term effects on the bladder. A longitudinal study of 121 children with neurogenic bladder treated for a median duration of 19 months found that oral oxybutynin had sustained effects on both continence and bladder compliance. Of the 51 children with a pretreatment EFP of >40 cm/H20, mean EFP decreased to and remained <40 cm/H20 in 63 % throughout treatment. Oxybutynin was well tolerated with only six discontinuations due to AEs [32].
As an alternative route of administration, intravesical oxybutynin has also been evaluated for its potential to decrease the side effects of anticholinergic therapy by reducing first pass metabolism in the liver while maintaining high systemic efficacy and bioavailability [33–36]. A recent publication reported 15-year mean follow-up following transition from oral to intravesical oxybutynin for pediatric NGB in ten children with DSD. Ongoing suppression of detrusor overactivity, maintenance of long-term effects on bladder compliance (30 % at onset versus 90 % at last follow-up had an EFP <40 cm/H20) and increased bladder capacity (from 5th to 25–50th percentile for age) was observed. Intravesical oxybutynin was well-tolerated; no side effects were reported [37••].
Finally, medication alternatives to anticholinergic therapy are being evaluated. A recent study highlighted the potential for further targeting of the adrenergic pathway by finding an association between children whose LUTS failed to respond to anticholinergics and genetic polymorphisms in the adrenergic rather than cholinergic pathway [38]. An example of an alternative agent that targets adrenergic transmission is mirabegron, a β3 agonist demonstrated to have efficacy in adults with NDO due to SCI with significant decreases in EFP, frequency of evacuation and incontinence episodes [39]. Although anticholinergic therapy is currently the mainstay of medical management for pediatric NGB, further studies may provide additional options for medical management, including the potential for targeted pharmacologic manipulation of the adrenergic pathway in children with NDO.
Intravesical Botulinum Toxin A
Botulinum toxin A was FDA approved in adults for intravesical injection in the treatment of urinary incontinence due to NDO. Prospective assessments in children with NGB have likewise demonstrated significant improvement in continence, bladder capacity and compliance following Botox injection [40, 41]. In addition, a decrease in fibrosis after multiple injections has been described that may correspond to the potential for inhibition of detrimental remodeling in certain bladders [42].
Two retrospective series recently explored outcomes in the treatment of pediatric NGB and optimization of patient selection for intravesical Botox therapy. Khan et al. reviewed the experience at a single center of children with NDO who were either anticholinergic refractory or intolerant [43•]. Following injection of 300U into the detrusor, 54 % of children reported improved continence. A corresponding increase in mean cystometric capacity and a decrease in EFP and frequency of uninhibited detrusor contractions were observed. Mean duration of clinical effectiveness was 4.6 months (range 0–18). Of note, continence rates appeared to be highest in the subset of children with anticholinergic intolerance (75 %) versus those refractory to medical management (50 %) following Botox injection. Although interpretation remains inconclusive as the number within the cohort intolerant of anticholinergic therapy was small, it was hypothesized that these children may represent a subset less likely to have a fibrotic bladder [43•]. This observation aligns with publications by Tiryaki [44], Kim [45], and Kask et al. [46] which all found that severely impaired bladder compliance, particularly in the presence of a lack of detrusor activity, portends the poorest prognosis for response to intravesical botox injections in children with NGB. In these series, children with NDO and mild to moderate changes in compliance had a better response both in terms of continence and bladder dynamics following intravesical botox injection as compared to those with more severe compliance changes.
Regardless of the efficacy of a single intravesical Botox treatment for these children, however, a follow-up question recently addressed was its utility as a chronic management strategy. In 22 children with NDO who underwent a total of 62 intravesical Botox injections over a 10-year period, the median response time was 7 months (range 0–25) with a stable response observed up to a 7th injection [47••]. This aligns with a former series of eight children with NGB whose pre and postoperative urodynamics demonstrated a mean EFP decrease to <40 cm/H20 and a consistent increase in bladder capacity after each of three repeated injections [48]. Although not currently FDA approved for treatment of NDO in children, Botox is a promising early alternative to augmentation, particularly for those individuals who are intolerant of anticholinergic therapy. Further studies are anticipated to continue to elucidate the optimal candidates, timing and utility of early treatment with Botox in children with NDO.
Surgical Reconstruction
When medical and intravesical options fail to provide satisfactory results, surgical reconstruction may be required to maintain low intravesical storage pressure and achieve treatment goals for urinary continence. Current options for surgical management include incontinent diversion for those who are not candidates for CIC or individualized combinations of augmentation cystoplasty (AC), a bladder outlet procedure such as bladder neck reconstruction (BNR), sling, artificial urethral sphincter or bladder neck closure (BNC) and creation of a catheterizable channel [10••]. In the past year, literature contributions included analyses of enterocystoplasty (EC) outcomes, the selection of children for bladder neck reconstruction without concurrent bladder augmentation and the expanding role of robotics in reconstructive surgery.
Outcomes Following Augmentation Cystoplasty
The most common tissue sources currently utilized for AC are autologous ileum or colon. Although typically effective in increasing bladder capacity and compliance, an EC is associated with both short- and long-term morbidity and requires lifelong urologic management. Two recent analyses of the American College of Surgeons’ National Surgical Quality Database (NSQIP) reported an approximately 30 % (23–33 %) 30-day overall event rate in children who underwent EC with or without appendicovesicostomy. The most common complications included urinary tract infections (9.6–10.7 %), wound complications (7.4–8.7 %), blood transfusions (6–6.1 %) and sepsis (2.8–3.5 %). Median length of stay was 8 days in both analyses with 30-day reoperative rates of up to 10 % and readmission rates of 13 % [49•, 50•]. In a separate study, when comorbidities were analyzed for contribution to perioperative outcomes in urologic bowel procedures, a BMI ≥95th percentile was found in 21 % of these children and was associated with both a fourfold increase in adjusted odds of overall wound complications [51] and an increased 30-day overall event rate [52].
In addition to short-term outcomes, 10-year cumulative complication incidence was calculated from the Pediatric Health Information System database in evaluation of 2831 augmentation cystoplasties. Causes of long-term morbidity included bladder rupture (2.9–6.4 %), small bowel obstruction (5.2–10.3 %), bladder stones (13.3–36 %) and pyelonephritis (16.1–37.1 %). Secondary surgery estimates included a 13.3–35.1 % rate of cystolitholapaxy and re-augmentation in 5.2–13.4 % [53]. In analysis of risk factors, an increased risk of bladder rupture and stone development was associated with bladder neck procedures and stoma creation at the time of augmentation [53].
Taken together, outcome studies such as these highlight both the importance of life-long urologic care following EC and the need for alternative management strategies. To date, bioengineered tissue alternatives have provided less than desirable human applicability with survival of large grafts limited in part by a lack of early vascularization leading to early functional loss and fibrosis [54, 55]. However, the significant morbidity associated with the use of autologous bowel for AC should continue to provide impetus for ongoing research to create viable tissue alternatives for these children.
Outcomes of Bladder Neck Procedures Without Augmentation Cystoplasty
In the National Spina Bifida Patient Registry database, less than one third of children with spina bifida at their baseline registry evaluation were continent of either urine or stool [28]. For children with minimal outlet resistance who have not achieved the desired continence result via medical management, the surgical solution most often offered historically was a concurrent bladder neck reconstructive procedure, catheterizable channel and augmentation cystoplasty. In an attempt to address the morbidity of EC, multiple series have recently questioned the necessity of bladder augmentation in all cases [56].
In three recent series with 2 to 9 years of follow-up, children who underwent isolated bladder neck procedures proceeded to augment between 12 and 45 % of the time [57••, 58•, 59•]. Unfortunately, regardless of methodology utilized for urodynamic testing, no definitive preoperative urodynamic parameters were identified that could have predicted the response of each bladder to increased outlet resistance and the need for subsequent bladder neck or augmentation procedures. In the largest series, 18 % of 109 children who underwent a bladder outlet procedure without augmentation followed for a mean of 4.9 years had proceeded to AC. Although upper tract hydronephrosis or VUR resolved in all children in this series following AC, most concerning was the presence of new or increased renal scarring observed in 21 % of children evaluated both before and after an isolated bladder outlet procedure. Furthermore, the authors reported an estimated 10-year cumulative incidence of AC in 30 %, with over 50 % having developed upper tract changes and 20 % diagnosed with chronic kidney disease. Although significantly associated with the incidence of new or increased postoperative renal scarring, preoperative bladder compliance did not correlate with long-term success overall [57••]. Putting these series together, although there are bladders with myogenic failure and adequate compliance that may maintain low intravesical pressure following an isolated bladder neck procedure, the ability to preoperatively select optimal candidates for BNR without augmentation remains elusive.
Robotic Approaches to Reconstructive Procedures
Surgical options continue to evolve with the application of a minimally invasive approach to an increasing number of reconstructive procedures. In the past year, several series have reported the feasibility of a robotic approach for AC, bladder neck reconstruction (BNR) and appendicovesicostomy. In a retrospective comparison of open (n = 13) versus robotic (15) ileocystoplasties with or without concomitant procedures, operative time was significantly longer (623 versus 287 min) while median length of stay was decreased (6 versus 8 days) in robotic as compared to open cohorts. Postoperative increase in bladder capacity, narcotic use and complication rates did not differ between the two approaches [60]. Similarly, feasibility was demonstrated of an entirely intracorporeal robotic EC with or without creation of catheterizable channels in a recent multi-institutional series of 22 adults [61]. Specific to the catheterizable channel, a single center experience of 39 robotic and 28 open appendicovesicostomies reported no difference in acute complication (26 and 29 %, respectively) or reoperation (29 versus 33 %) rates at a mean follow-up of 2.8 ± 2.5 years. However, the robotic series had higher rates of Clavien grade 2–3 complications including three early reoperations due to early bowel obstruction with internal hernia in the robotic cohort addressed by an altered technique with fixation of the channel and bladder to the abdominal wall [62]. Series such as these are needed to continue to define the long-term outcomes of robotic procedures with ongoing procedural optimization.
Robotic outcomes of bladder neck reconstruction have also recently been published. In one series, 38 robotic assisted Leadbetter-Mitchell type BNR and continent catheterizable channels without AC were performed. After a mean follow-up of 21 months, 82 % of individuals were dry with CIC which compares favorably with the 50–85 % continence rates published in the open literature [63]. In a second series, outcomes were compared between 19 robotic and 26 open bladder neck reconstructions. Operative time was significantly longer in the robotic cohort (8.2 versus 4.5 h) but no difference was observed in length of stay (median 4 days in each cohort) or acute complication rates (16 and 12 %, respectively). With a mean followup of 2.3 versus 3.2 years in the robotic versus open cohorts, there was no difference in rates of subsequent incontinence procedures performed in 42 and 56 % of children respectively [64].
As robotic procedures become increasingly common, recent studies have evaluated means to optimize perioperative care. A recent assessment of regional anesthesia options following robotic assisted procedures including transversus abdominal plane (TAP) and caudal blocks versus no regional block addressed these questions. A significant reduction in intraoperative opioid use and need for antiemetics was seen in children undergoing upper or lower tract urologic robotic surgery with a caudal block as compared to TAP or no regional anesthesia [65]. However, there was no significant difference in postoperative opioid use, maximum pain scores within 24 h postoperatively or length of hospital stay [65]. As surgical management options continue to evolve, ongoing optimization of surgical planning and perioperative management continues to be needed to refine techniques and outcomes for children with neurogenic bladder.
Achieving Long-Term Goals: Quality of Life Assessment and Transition of Care
To evaluate in a systematic way whether the goals of individuals with neurogenic bladder are being met, several quality of life assessment tools have recently been evaluated including QUALAS-A [66] and QUALAS-C [67••] designed for adults and children with spina bifida as well as adolescent specific bowel [68] and bladder [69] functional measurement instruments. Although a complex relationship exists, qualitative interviews of youth and parents published in the past year reiterated the effect of continence on quality of life through greater independence and opportunities for social participation reported in children with minimal versus higher volume incontinence [70]. Development of assessment, educational tools [71] and options for bladder emptying [72] continue to refine our understanding to better address the needs of children with neurogenic bladder through facilitation of independence in bowel and bladder management.
Children with neurogenic bladder represent one of the largest pediatric populations in need of complex ongoing urologic management as they transition to adult care. Several studies that recently evaluated both youth with neurogenic baldder and their providers have emphasized the need for specialized treatment availability. In a survey of urologists, the majority (81 %) recommended that a urologist with training in adolescent/transitional care and experience in performance of genitourinary reconstructive procedures is ideally suited for the care of the mature patient with a complex genitourinary history [73]. Individuals who had completed this transition of urologic care were in agreement with the benefits of specialized management with 95 % considering their visit to a transitional care clinic beneficial [74]. Thoughtful planning in this process including assistance in navigation of an adult healthcare program and coordination with specialists who have expertise in this area will help to promote long-term genitourinary health for individuals with neurogenic bladder.
Conclusion
The goals in management of the pediatric neurogenic bladder include preservation of the upper and lower urinary tracts and optimization of quality of life throughout childhood and in the transition to adulthood. As highlighted in this review of literature published in the past year, the techniques of assessment, medical and surgical management continue to evolve. Ongoing research to improve understanding of outcome determinants and optimal choice of candidates for each management strategy continues to be needed to minimize the significant current impact of the pediatric neurogenic bladder.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Parker SE MC, Canfield MA, Rickard R, National Birth Defects Network, et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin MolTeratol. 2010;88(12):1008–16.
Lloyd JC, Wiener JS, Gargollo PC, Inman BA, Ross SS, Routh JC. Contemporary epidemiological trends in complex genitourinary anomalies. J Urol. 2013;190(4 Suppl):1590–5.
Sutton LN, Adzick NS, Bilaniuk LT, Johnson MP, et al. Improvement in hindbrain herniation demonstrated by serial fetal magnetic resonance imaging. JAMA. 1999;282(19):1828–31.
Clayton DB, Tanaka ST, Trusler L, Thomas JC, et al. Long-term urological impact of fetal myelomeningocele closure. J Urol. 2011;186(4 Suppl):1581–5.
Lee NG, Gomez P, Uberoi V, Kokorowski PJ, et al. In utero closure of myelomeningocele does not improve lower urinary tract function. J Urol. 2012;188(4 Suppl):1567–71.
Adzick NS, Thom EA, Spong CY, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1004.
Brock JW, Carr MC, Adzick NS, Burrows PK, et al. Bladder function after fetal surgery for myelomeningocele. Pediatrics. 2015;136(4):906–13. This study presented urologic function at 12 and 30 months following a randomized prospective multi-institutional trial (MOMS) of prenatal versus neonatal closure for open myelomeningocele. No difference was observed between the two cohorts in the primary endpoint of death or meeting criteria for clean intermittent catheterization at 30 months of age.
da Cruz ML, Liguori R, Garrone G, Leslie B, et al. Categorization of bladder dynamics and treatment after fetal myelomeningocele repair: first 50 cases prospectively assessed. J Urol. 2015;193(5):1808–12.
Carr M. Urological results after fetal myelomeningocele repair in pre-MOMS trial patients at the Children’s Hospital of Philadelphia. Fetal Diagn Ther. 2015;37(3):211–8.
SnowLisy DC, Yerkes EB, Cheng EY. Update on urological management of spina bifida from prenatal diagnosis to adulthood. J Urol. 2015;194:288–96. This review provided an overview of recent literature evaluating the urologic management of spina bifida with an emphasis on outcomes following an expectant versus proactive approach to management. The authors concluded that while literature supports both approaches to protect children from renal injury, an expectant approach may increase long-term rates of bladder augmentation.
Shiroyanagi Y, Suzuki M, Matsuno D, Yamazaki Y. The significance of 99mtechnetium DMSA renal scan in children with spina bifida during long-term followup. J Urol. 2009;181(5):2262–6.
Cohen RA, Rushton HG, Belman AB, Kass EJ, et al. Renal scarring and vesicoureteral reflux in children with myelodysplasia. J Urol. 1990;144(2 Pt 2):541–5.
Leonardo CR, Filgueiras MF, Vasconcelos MM, Vasconcelos R, et al. Risk factors for renal scarring in children and adolescents with lower urinary tract dysfunction. Pediatr Nephrol. 2007;22(11):1891–6.
DeLair SM, Eandi J, White MJ, Nguyen T, Stone AR, Kurzrock EA. Renal cortical deterioration in children with spinal dysraphism: analysis of risk factors. J Spinal Cord Med. 2006;30(Supp 1):30–4.
Veenboer PW, Hobbelink MG, Ruud Bosch JL, Dik P, van Asbeck FW, Beek FJ, et al. Diagnostic accuracy of Tc-99m DMSA scintigraphy and renal ultrasonography for detecting renal scarring and relative function in patients with spinal dysraphism. Neurourol Urodyn. 2015;34(6):513–8. 122 adults with spinal dysraphism who presented to a specialized clinic were prospectively evaluated with both a DMSA nuclear scan and a renal US. Significantly more renal scars were detected on DMSA with poor correlation between findings of the two radiographic tests.
Bush NC, Keays M, Adams C, Mizener K, Pritzker K, Smith W, et al. Renal damage detected by DMSA despite normal renal ultrasound in children with febrile UTI. J Pediatr Urol. 2015;11(3):126e.1. 7.
Logvinenko T, Chow JS, Nelson CP. Predictive value of specific ultrasound findings when used as a screening test for abnormalities on VCUG. J Pediatr Urol. 2015;11(4):176.e1–7.
Sturm RM, Cheng EY. Bladder wall thickness in the assessment of neurogenic bladder: a translational discussion of current clinical applications. Ann Transl Med. 2016;4(2):32–7.
Silva JA, Gonsalves MD, de Melo RT, Carrerette FB, Damiao R. Association between the bladder wall thickness and urodynamic findings in patients with spinal cord injury. World J Urol. 2015;33(1):131–5.
Sekerci CA, İşbilen B, Isman F, et al. Urinary NGF, TGFb1, TIMP2 and bladder wall thickness predict neurourological findings in children with myelodysplasia. J Urol. 2014;191:199–205.
Tanaka H, Matsuda M, Moriya K, et al. Ultrasonographic measurement of bladder wall thickness as a risk factor for upper urinary tract deterioration in children with myelodysplasia. J Urol. 2008;180:312–6.
Muller L, Abrahamsson K, Sillen Y, et al. Ultrasound assessment of detrusor thickness in children and young adults with spina bifida. J Urol. 2006;175:704–8.
Kim WJ, Shiroyanagi Y, Yamazaki Y. Can bladder wall thickness predict videourodynamic findings in children with spina bifida? J Urol. 2015;194(1):180–3. Ultrasonographic measurement of bladder wall thickness of 53 children with spina bifida including 31 at specific cystometric capacities was obtained. Although specific aspects of methodology and a closely managed study population may have contributed to the outcome, no significant association was observed between BWT and high-risk urodynamic parameters.
Yamada S, Iacono RP, Andrade T, Mandybur G, Yamada BS. Pathophysiology of tethered cord syndrome. Neurosurg Clin N Am. 1995;6:311–23.
Alzahrani A, Alsowayan O, Farmer JP, Capolicchio JP, Jednak R, El-Sherbiny M. Comprehensive analysis of the clinical and urodynamic outcomes of secondary tethered spinal cord before and after spinal cord untethering. J Pediatr Urol. 2015.
Frainey BT, Yerkes EB, Menon VS, Gong EM, Meyer TA, Bowman RM, et al. Predictors of urinary continence following tethered cord release in children with occult spinal dysraphism. J Pediatr Urol. 2014;10(4):627–33.
Yener S, Thomas DT, Hicdonmez T, Dagcinar A, Bayri Y, Kaynak A, et al. The effect of untethering on urologic symptoms and urodynamic parameters in children with primary tethered cord syndrome. Urology. 2015;85(1):221–6.
Sawin KJ, Liu T, Ward E, Thibadeau J, et al. The national spina bifida patient registry: profile of a large cohort of participants form the first 10 clinics. J Pediatr. 2015;166(2):444–50.
Kavoussi LR, Novick AC, Partin AW, Peters CA, Campbell Walsh Urology. 10th ed, ed. W. AJ. 2012: Elsevier.
Schlomer BJ, Saperston K, Baskin L. National trends in augmentation cystoplasty in the 2000s and factors associated with patient outcomes. J Urol. 2013;190(4):1352–8.
Szymanski KM, Misseri R, Whittam B, Adams CM, Kirkegaard J, King S, et al. Mortality after bladder augmentation in children with spina bifida. J Urol. 2015;193(2):643–9.
Lee JH, Kim K, Lee YS, Han SW, Kim KS, Song SH, et al. Efficacy, tolerability and safety of oxybutynin chloride in pediatric neurogenic bladder with spinal dysraphism. Korean J Urol. 2014;55(12):828–33.
Buyse G, Waldeck K, Verpoorten C, et al. Intravesical oxybutynin for neurogenc bladder dysfunction: less systemic side effects due to reduced first pass metabolism. J Urol. 1998;160:892–6.
Krause P, Fuhr U, Schnitker J, Albrecht W, et al. Pharmacokinetics of intravesical versus oral oxybutynin in healthy adults: results of an open label, randomized, prospective clinical study. J Urol. 2013;190(5):1791–7.
Buyse G, Verpoorten C, Vereecken R, et al. Intravesical application of a stable oxybutynin solution improves therapeutic compliance and acceptance in children with neurogenic bladder. J Urol. 1998;160:1084–7.
Lazarus J. Intravesical application of a stable oxybutynin in the pediatric neurogenic bladder. Nat Rev Urol. 2009;6:671–4.
Humblet M, Verpoorten C, Christiaens MH, Hirche H, et al. Long-term outcome of intravesical oxybutynin in children with detrusor-sphincter dyssynergia: with special reference to age-dependent parameters. Neurourol Urodyn. 2015;34:336–42. Long-term (15 year) followup after intravesical oxybutynin administration was reported in 10 children with detrusor-sphincter dyssynergia. Intravesical oxybutynin was well tolerated with prolonged effects on compliance, capacity and suppresion of detrusor activity.
Gurocak S, Konac E, Ure I, Senol C et al. The impact of gene polymorphisms on the success of anticholinergic treatment in children with overactive bladder. Disease Markers. 2015:732686
Wollner J, Pannek J. Initial experience with the treatment of neurogenic detrusor overactivity with a new β-3 agonist (Mirabegron) in patients with spinal cord injury. Spinal Cord. 2016;54:78–82.
Riccabona M, Koen M, Schindler M, Goedele B, Pycha A, Lusuardi L, et al. Botulinum-A toxin injection into the detrusor: a safe alternative in the treatment of children with myelomeningocele with detrusor hyperreflexia. J Urol. 2004;171(2 Pt 1):845–8.
Figueroa V, Romao R, Pippi Salle JL, Koyle MA, et al. Single-center experience with botulinum toxin endoscopic detrusor injection for the treatment of congenital neuropathic bladder in children. J Pediatr Urol. 2014;10(2):368–73.
Pascali MP, Mosiello G, Boldrini R, Salsano ML, Castelli E, Gennaro MD. Effects of botulinum toxin type A in the bladder wall of children with neurogenic bladder dysfunction: a comparison of histological features before and after injections. J Urol. 2011;185(6 Suppl):2552–7.
Khan MK, VanderBrink B, DeFoor WR, Minevich E, et al. Botulinum toxin injection in the pediatric population with medically refractory neuropathic bladder. J Pediatr Urol, 2015. pending publication: p. 1-6. This was a retrospective series of 22 children with neurogenic bladders who were either refractory or intolerant to anticholinergics and proceeded to intravesical botox inejctions. This study evaluated predictive criteria for the response to botox injection and proposed that bladders with the highest degrees of fibrosis may be least responsive to this therapeutic option.
Tiryaki S, Yagmur I, Parlar Y, Ozel K, et al. Botulinum injection is useless on fibrotic neuropathic bladders. J Pediatr Urol. 2015;11(27):1.e1–27.e4.
Kim SW, Choi J, Lee YS, Han SW, Im YJ. Preoperative urodynamic factors predicting the outcome of botulinum toxin-A intradetrusor injection in children with neurogenic detrusor overactivity. J Urol. 2014;84(6):1480–4.
Kask M, Rintala R, Taskinen S. Effect of onabotulinumtoxinA treatment on symptoms and urodynamic findings in pediatric neurogenic bladder. J Pediatr Urol. 2014;10:280–3.
Greer T, Abbott J, Breytenbach W, McGuane D, et al, Ten years of experience with intravesical and intrasphincteric onabotulinumtoxinA in children. J Pediatr Urol, 2015. pending publication: p. 1.e1-1.e6. This retrospective series evaluated 53 children who received multiple intravesical or intrasphincteric botox injections for varied indications. In a subset, sustained responses were observed to intravesical botox for NDO over a 10-year observation period. Additionally, 45% of children with dysfunctional voiding or DSD who received a single injection of intrasphincteric botox had a prolonged clinical response.
LeNue R, Harper L, DeSeze M, Bouteiler C, et al. Evolution of the management of acquired neurogenic bladder in children using intradetrusor botulinum toxin type A injections: 5-year experience and perspectives. J Pediatr Urol. 2012;8:497–503.
Mcnamara ER, Kurtz M, Schaeffer AJ, Logvinenko T, Nelson CP. 30-Day morbidity after augmentation enterocystoplasty and appendicovesicostomy: a NSQIP pediatric analysis. J Pediatr Urol. 2015;11:209.e1–6. This study analyzed short-term outcomes following augmentation enterocystoplasty and/or appendicovesicostomy in children from a large national sample (NSQIP) in the United States between 2012-2013. In this series of 461 patients, the composite measure of any 30-day event occurred in 28% of the cohort and was associated with surgical risk score, longer operative time and increased number of concurrent procedures.
Du K, Mulroy E, Wallis MC, Zhang C, Presson AP, Cartwright PC. Enterocystoplasty 30-day outcomes from National Surgical Quality Improvement Program Pediatric 2012. J Pediatr Surg. 2015;50:1535–9. In this NSQIP analysis results of enterocystoplasty with or without appendicovesicostomy were provided in 2012. Outcomes were similar to those reported above. However, addition of an appendicovesicostomy or BNR were not associated with a significant increase in complication rates.
Kurtz MP, McNamara E, Schaeffer AJ, Logvinenko T, Nelson CP. Association of BMI and pediatric urologic postoperative events: results from pediatric NSQIP. J Pediatr Urol. 2015;11:224e.1–e.6.
McLeod DJ, Asti L, Mahida JB, Deans KJ, Minneci PC, Preoperative risk assessment in children undergoing major urologic surgery. J of Pediatr Urol, 2015. epub ahead of print
Schlomer BJ, Copp HL. Cumulative incidence of outcomes and urologic procedures after augmentation cystoplasty. J Pediatr Urol. 2014;10:1043–50.
Osborn SL, Kurzrock E. Bioengineered bladder tissue—close but yet so far! J Urol. 2015;194(3):619–20.
Gill BC, Damaser M, Chermansky CJ. Future perspectives in bladder tissue engineering. Curr Bladder Dysfunct Rep. 2014;10(4):443–8.
Dave S, Salle PJ, Lorenzo AJ, Braga LHP, et al. Is long-term bladder deterioration inevitable following successful isolated bladder outlet procedures in children with neuropathic bladder dysfunction? J Urol. 2008;179:1991–6.
Grimsby GM, Menon V, Schlomer BJ, Baker LA, et al. Long-term outcomes of bladder neck reconstruction without augmentation cystoplasty in children. J Urol. 2016;195:155–61. In this 109 patient retrospective series of varied bladder neck procedures followed for a mean of 4.9 years, 54% underwent secondary continence procedures, 18% proceeded to augmentation cystoplasty. Nearly half developed VUR or hydronephrosis and 21% renal scarring during the study period. No preoperative findings on urodynamics predicted the need for delayed augmentation although a history of vesicostomy or VUR were significnat associations.
Snodgrass W, Granberg C, Clinical indications for augmentation in children with neurogenic urinary incontinence following bladder outlet procedures: results of a 14-year observational study. J Pediatr Urol, 2016. published ahead of print: p. 1.e1-8. This 82 patient retrospective series demonstrated feasibility and revision of surgical techniques over time in the use of a Leadbetter/Mitchell bladder neck revision with sling as compared to later use of a bladder neck sling alone that significantly improved continence outcomes in the absence of augmentation cystoplasty. While 12% of children in this series after a mean followup of 60 months proceeded to augmentation cystoplasty, no preoperative UDS parameter predicted need for subsequent augmentation.
Whittam B, Szymanski K, Misseri R, Carroll A, Kaefer M, Rink R, et al. Long-term fate of the bladder after isolated bladder neck procedure. J Pediatr Urol. 2014;10:886–91. In this retrospective series of 29 individuals who underwent bladder neck procedrues followed for a mean of 8.9 yearss, 45% proceeded to a delayed augmentation cystoplasty. Although preoperative UDS findings did not correlate with outcomes, those who underwent delayed augment had smaller capacity bladders and poorer compliance following BNR.
Murthy P, Cohn J, Seliq RB, Gundeti MS. Robot-assisted laparoscopic augmentation ileocystoplasty and mitrofanoff appendicovesicostomy in children: updated interim results. Eur Urol. 2015;68(6):1069–75.
Flum AS, Zhao L, Kielb SJ, Wilson EB, Shu T, Hairston JC. Completely intracorporal robotic-assisted laparoscopic augmentation enterocystoplasty with continent catheterizable channel. Urology. 2014;84(6):1314–8.
Grimsby GM, Jacobs M, Gargollo PC. Comparison of complications of robot-assisted laparoscopic and open appendicovesicostomy in children. J Urol. 2015;194(3):772–6.
Gargollo PC. Robotic-assisted bladder neck repair: feasibility and outcomes. Urol Clin North Amer. 2015;42(1):111–20.
Grimsby GM, Jacobs M, Menon V, Schlomer BJ, Gargollo PC, Perioperative and short-term outcomes of robotic versus open bladder neck procedures in patients with neurogenic incontinence. J Urol, 2015. Epub ahead of print: p. 1-5.
Faasse MA, Lindgren B, Frainey BT, Marcus CR, Szcodry DM, Glaser AP, et al. Perioperative effects of caudal and transversus abdominis plane (TAP) blocks for children undergoing urologic robot-assisted laparoscopic surgery. J Pedatr Urol. 2015;11(3):121.e1–e7.
Szymanski KM, Misseri R, Whittam B, Raposo SM, King SJ, Kaefer M, et al. Quality of life assessment in spina bifida for adults (QUALAS-A): development and international validation of a novel health-related quality of life instrument. Qual Life Res. 2015;24(10):2355–64.
Szymanski KM, Misseri R, Whittam B, Yang DY, Raposo SM, King S, et al. Quality of life assessment in spina bifida for children (QUALAS-C): development and validation of a novel health-related quality of life instrument. Urology. 2016;87:178–84. This study described the development and validation of QUALAS-C which is a brief questionnaire developed in 8 to 12 year old children with spina bifida in the assessment of health related quality of life, bowel and bladder function.
Hubert KC, Sideridis G, Sherlock R, Queally J, Rosoklija I, Kringle G, et al. Validation of a bowel dysfunction instrument for adolescents with spina bifida. J Pediatr Urol. 2015;11(4):199.e1–e7.
Hubert KC, Sideridis G, Sherlock R, Rosoklija I, Kringle G, Johnson K, et al. Urinary incontinence in spina bifida: initial instrument validation. Res Dev Disabil. 2015;40:42–50.
Fischer N, Church P, Lyons J, McPherson AC. A qualitative exploration of the experiences of children with spina bifida and their parents around incontinence and social participation. Child Care Health Dev. 2015;41(6):954–62.
Holland JE, DeMaso D, Rosoklija I, Johnson KL, Manning D, Bellows AL, et al. Self-cathing experience journal: enhancing the patient and family experience in clean intermittent catheterization. J Pediatr Urol. 2015;11(4):187.e1–6.
Sturm R, Y.J., Durbin-Johnson B, Kurzrock E, Use of a diurnal indwelling catheter to improve quality of life for patients with spinal cord disorders, in ESPU. 2015: Prague.
Szymanski KM, Misseri R, Whittam B, Large T, Cain MP. Current opinions regarding care of the mature pediatric urology patient. J Pediatr Urol. 2015;11(5):251.e1–e4.
Shalaby MS, Gibson A, Granitsiotis P, Conn G, Cascio S. Assessment of the introduction of an adolescent transition urology clinic using a validated questionnaire. J Pediatr Urol. 2015;11(2):89.e1–e5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Cheng Reports other from Allergan, Inc. outside the submission
Dr Sturm declare that they have no conflicts of interest
Human and Animal Rights and Informed Consent
This article does not contain studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Pediatric Bladder Dysfunction
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sturm, R.M., Cheng, E.Y. The Management of the Pediatric Neurogenic Bladder. Curr Bladder Dysfunct Rep 11, 225–233 (2016). https://doi.org/10.1007/s11884-016-0371-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-016-0371-6