Abstract
Recent studies suggested that allergic disorders and increased eosinophil count were associated with atherosclerosis. The purpose of this study was to assess the relationship between eosinophil count and coronary artery calcification (CAC). We performed a cross-sectional study in 1363 consecutive participants with clinical suspicion of coronary heart disease (CHD). We evaluated the relationships between CAC score determined by multislice CT and peripheral eosinophil count as well as major cardiovascular risk factors, including age, body mass index, smoking status, hypertension, dyslipidemia, diabetes mellitus (DM), high-sensitivity C-reactive protein and estimated glomerular filtration rate (eGFR). Sex (P=0.0004), hypertension (P=0.0002), dyslipidemia (P=0.0004) and DM (P=0.0061) were associated with log(CAC+1), respectively. Positive correlations were found between log(CAC+1), and age (r=0.325, P<0.0001) and eosinophil count (r=0.165, P<0.0001). Negative correlations were found between log(CAC+1) and eGFR (r=−0.166, P<0.0001). Multivariate linear regression analysis demonstrated that age (β=0.314, P<0.0001), sex (β=0.124, P<0.0001), hypertension (β=0.084, P=0.0008), DM (β=0.108, P<0.0001), eGFR (β=−0.079, P=0.0021) and eosinophil count (β=0.147, P<0.0001) were independent determinants of log(CAC+1). In conclusion, eosinophil count correlated positively with CAC in participants with clinical suspicion of CHD.
Similar content being viewed by others
Introduction
Despite the availability of effective preventive therapies, cardiovascular disease remains a leading cause of morbidity and mortality. In addition to elevated lipoproteins and various coagulation factors, inflammatory mechanisms play a crucial role in the pathogenesis of atherosclerosis.1, 2 Moreover, allergic disorders such as allergic rhinitis or asthma have also been reported to be associated with atherosclerosis.3
The coronary artery calcification (CAC) score has recently been developed as a marker of coronary atherosclerosis, which can be assessed noninvasively using multislice CT (MSCT). CAC is an established quantitative, objective measure of coronary artery atherosclerosis, and several studies have revealed a correlation between CAC and angiographic stenosis.4, 5 Moreover, CAC scores have been shown to be related to coronary heart disease (CHD) risk factors and cardiovascular events.6, 7 In this study, we examined the relationship between eosinophil count in peripheral blood and CAC score determined by MSCT.
Methods
Subjects and study design
We performed a cross-sectional study in 1363 consecutive participants with clinical suspicion of CHD, who visited the Department of Cardiology, Yamashiro Public Hospital (Kyoto, Japan) from April 2006 to December 2009. Contraindications to participation in this study were known hemodynamic instability, previous coronary artery bypass surgery or percutaneous coronary intervention and possible pregnancy. Participants were also excluded when they were taking any medications that are known to affect allergic reaction (for example, corticosteroid, antiallergy agents).
All participants provided details of their demographics, medical history and medication usage at the time of CAC screening. Body mass index was calculated as weight in kg divided by height in m2. Smoking was defined as current tobacco usage. Hypertension was defined as systolic blood pressure ⩾140 mm Hg, diastolic blood pressure ⩾90 mm Hg and/or having received treatment for hypertension. Dyslipidemia was defined as a total cholesterol concentration ⩾5.7 mmol l−1, a triglyceride concentration ⩾1.7 mmol l−1 and/or having received treatment for dyslipidemia. Diabetes mellitus (DM) was defined as fasting plasma glucose ⩾7.0 mmol l−1 and/or a current history of antidiabetic medication. The study protocol was approved by the local investigational review board committee, and conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution′s human research committee. Signed informed consent was obtained from all subjects.
Laboratory data
In the morning, after an overnight fast, 10 ml of venous blood was collected for the measurement of the levels of creatinine, high-sensitivity C-reactive protein (hs-CRP), total cholesterol, triglyceride and fasting plasma glucose. Estimated glomerular filtration rate (eGFR) was used to estimate kidney function using the abbreviated Modification of Diet in Renal Disease equation, which includes variables for age, sex, race and serum creatinine.8 Peripheral leukocyte analyses included total leukocyte counts and percentages of eosinophils using an automated cell counter. The absolute count of eosinophil was calculated as the product of its percentage and total leukocyte count.
Measurement of CAC score
We performed MSCT (Aquillion 64, Toshiba Medical, Tokyo, Japan). Calcification scoring parameters were 2 mm collimation width, a gantry rotation speed of 0.4 s/rotation, 120 kV and 100 mA. During a single breath hold, images of the heart, from the level of the tracheal bifurcation to below the base of the heart, were acquired using prospective ECG triggering at 50% of the RR interval. Total CAC scores were determined on a workstation (ZIO Station, ZIO Soft, Inc., Tokyo, Japan) with software for CAC according to the Agatston method as previously described.9 CAC was defined on CT images as the presence of more than two contiguous pixels with greater than 130 Hounsfield units. The Agatston calcium score was obtained by multiplying the area by a weighting factor that depends on the peak signal anywhere in the lesion.
MSCT Image Reconstruction
A bolus of 50 ml contrast agent (Iomeron 350, Eizai Co., Tokyo, Japan) was injected intravenously at a rate of 4.0 ml s−1. As soon as the signal density level in the ascending aorta reached a predefined threshold of 100 Hounsfield units, acquisition of the CT data and the ECG trace were started. The volume data set for coronary artery imaging was acquired in spiral mode, with a collimation of 64 × 0.5 mm, a gantry rotation of 400 ms, helical pitch of 3.2, tube energy of 120 kV and an effective tube current of 400 mA. The subject's ECG was digitized and monitored continuously during image acquisition. The raw data from the scans were reconstructed using a segment algorithm in all subjects. The reconstructed image data from the MSCT angiography were transferred to a computer workstation for post processing. Two experienced observers who were blinded to the subject’s identity and clinical presentation analyzed MSCT images. Arterial stenosis that produced more than 50% luminal narrowing was considered significant.
Statistical analysis
The statistical analyses were performed using the JMP version 8.0. software (SAS Institute Inc., Cary, NC, USA). A P value < 0.05 was considered statistically significant. Skewed variables were preliminarily log-transformed to improve the approximation to a Gaussian distribution and CAC scores were log-transformed after adding 1. Continuous variables are presented as the mean value ±1 s.d. and categorical variables are presented as number (percentage). Unpaired Student's t-tests were conducted to assess statistical significance of differences between groups. Continuous variables were compared among the groups by analysis of variance. A Tukey–Kramer post-hoc analysis was performed to determine significant differences among each group. The relationships between log(CAC+1) and eosinophil count or other variables were examined by Pearson's correlation analyses. To examine the effects of various factors on log(CAC+1), the following factors were considered simultaneously as independent variables for multivariate linear regression analysis: age, sex, body mass index, smoking status, hypertension, dyslipidemia, DM, hs-CRP, eGFR, total leukocyte count and eosinophil count. As the optimal cut-off point for eosinophil count in predicting CAC >0, CAC >100, CAC >400 or CAC >1000, we chose the point on the receiver operating characteristic (ROC) curve, which represented the largest sum of sensitivity and specificity. The ability to identify CAC >0, CAC >100, CAC >400 or CAC >1000 correctly by eosinophil count was measured as area under the ROC curve, sensitivity and specificity.
Results
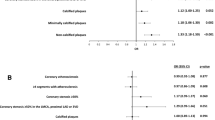
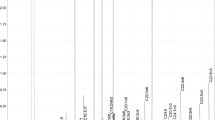
Table 1 shows selected characteristics of all participants (772 male, 591 female, aged 68. 0±11.0 years, range 23–96 years). Mean CAC and eosinophil count were 346.2 and 155.2 (106 per l), respectively. The correlation coefficients of the CAC scores for intraobserver reproducibility and interobserver reproducibility were observer1: 0.958 (P<0.0001), observer2: 0.941 (P<0.0001) and 0.947 (P<0.0001), respectively. Sex (P<0.0001), smoking status (P=0.0459) and significant stenosis (P=0.0034) were associated with eosinophil count, respectively (Table 2). Sex (P=0.0004), hypertension (P=0.0002), dyslipidemia (P=0.0004 ), DM (P=0.0061) and significant stenosis (P<0.0001) were associated with log(CAC+1), respectively. The eosinophil count quartiles were significantly associated with log (CAC+1) (P<0.0001), and the highest eosinophil count quartile (208.1–1180.0) had higher log (CAC+1) compared with the lowest (0–62.9)(P<0.0001) and second (63.0–120.5)(P=0.0001) eosinophil count quartiles. Positive correlations were found between log(CAC+1), and age (r=0.325, P<0.0001) and eosinophil count (r=0.165, P<0.0001) (Table 3). Negative correlations were found between log(CAC+1) and eGFR (r=−0.166, P<0.0001). No correlations were found between log(CAC+1) and body mass index, hs-CRP and total leukocyte count. No correlations were found between eosinophilic count and age (r=0.003, P=0.9214) or eGFR (r=−0.031, P=0.2564). Multivariate linear regression analysis demonstrated that age (β=0.314, P<0.0001), sex (β=0.124, P<0.0001), hypertension (β=0.084, P=0.0008), DM (β=0.108, P<0.0001), eGFR (β=−0.079, P=0.0021) and eosinophil count (β=0.147, P<0.0001) were independent determinants of log(CAC+1) (Table 3). Area under the ROC curve for eosinophil count predicting CAC >0, CAC >100, CAC >400 or CAC >1000 are presented in Figure 1. Furthermore, the optimal cut-off points, sensitivity and specificity according to the ROC curve for CAC >0, CAC >100, CAC >400 or CAC >1000 are also shown in Figure 1.
Discussion
Our study demonstrated that eosinophil count correlated positively with CAC. Multivariate linear regression analysis also identified eosinophil count as an independent determinant of log(CAC+1). Previous epidemiologic and clinical studies have suggested increased eosinophil count as a risk factor for coronary artery disease.10, 11, 12 In addition, Erdogan et al.13 reported a significant increase in the number of eosinophils in peripheral blood in patients with unstable angina pectoris compared with that in control subjects. However, to our knowledge this is the first report to investigate the relationship between eosinophil count and CAC, which suggests new avenues for research into the pathogenesis of CAC.
The pathogenesis of atherosclerosis is not well understood and remains a subject of debate. To explain the relationship between eosinophil count and CAC, several mechanisms can be suggested. Eosinophils are engaged in inflammatory reactions and are subjected to a process of cellular activation.14 Eosinophils synthesize and release bioactive mediators such as leukotriene C4, a potent stimulant of vasoactivity and smooth muscle contraction. Besides the direct activities of these eosinophil-derived mediators, eosinophils can induce the release of a number of vasoactive substances, including histamine, prostaglandin D2, and leukotrienes C4 and D4, from mast cells and basophils. Hallgren R15 suggested that the raised levels of eosinophil cationic protein in serum of patients with acute myocardial infarction are probably because of the active participation of eosinophils in the inflammatory process. In addition, major basic protein or eosinophil cationic protein, which is an eosinophil granule protein, activates platelets and promotes thrombus formation by inhibiting the function of thrombomodulin in hypereosinophic syndrome or allergic disease.16, 17 Rohrbach et al.18 reported that major basic protein and eosinophilic peroxidase activate platelets. Emanuele et al.19 suggested that increased eotaxin levels, an eosinophil-specific chemoattractant, are associated with the presence of coronary artery disease and that circulating levels of this chemokine may reflect the extent of coronary atherosclerosis. Besides, Niccoli et al.20 reported the association between eosinophil cationic protein levels, a sensitive marker of eosinophil activation, with plaque growth but not with plaque instability. Eosinophil cationic protein upregulates ICAM-1 expression on endothelial cells21, allowing adhesion of monocytes on endothelium, which is known to be a fundamental step in atherogenesis. In addition, Tintut et al.22 reported that monocytes enhance osteoblastic differentiation of calcifying vascular cells and enhance in vitro vascular calcification. Taking these findings together, it seems plausible that eosinophils correlate endothelial inflammation and atherosclerosis. With improved understanding of the critical role of inflammation in atherothrombosis23, attention has been focused on the inflammatory biomarker hs-CRP as a risk marker. Numerous epidemiologic studies have demonstrated an association of hs-CRP levels with increased risk of myocardial infarction, stroke, sudden cardiovascular death and peripheral vascular disease.24 However, our study did not indicate hs-CRP as an independent determinant of log(CAC+1).
The clinical relevance relates to potential preventive and therapeutic approaches, whereas the diagnostic relevance concerns the diagnostic utility of eosinophil count, as a provisional new marker of CAC, that can be measured easily in the clinical laboratory and applied in medical practice. In addition, our data suggest a possible link between allergic disease, as manifested by elevated eosinophil count, and CAC. The interesting concept of a role for eosinophils in CAC holds great promise for the development of new preventive measures involving antiallergy agents. Large prospective trials are needed to better assess the effects of allergic disorders on CAC.
Study Limitations
Limitations of our study include a cross-sectional design, which does not permit determination of causality. To our knowledge, this is the first study to investigate the association between eosinophil count and CAC. Although we are unable to determine whether eosinophil has a causative effect, these findings suggest that eosinophilia might be associated with an increased risk for the development and progression of CAC. Besides, in this study, participants were fairly homogenous in the sense that they were highly motivated to assess their CHD risk and had symptoms or clinical signs of CHD at the time of the examination.
Conclusions
Eosinophil count correlated positively with CAC in participants with clinical suspicion of CHD. In other words, our data might present evidence for a possible link between allergic disease, as manifested by elevated eosinophil count, and CAC.
References
De Servi S, Mazzone A, Ricevuti G, Fioravanti A, Bramucci E, Angoli L, Stefano G, Specchia G . Granulocyte activation after coronary angioplasty in humans. Circulation 1990; 82: 140–146.
Wick G, Knoflach M, Xu Q . Autoimmune and inflammatory mechanisms in atherosclerosis. Annu Rev Immunol 2004; 22: 361–403.
Togias A . Systemic effects of local allergic disease. J Allergy Clin Immunol 2004; 113: 8–14.
Baumgart D, Schmermund A, Goerge G, Haude M, Ge J, Adamzik M, Sehnert C, Altmaier K, Groenemeyer D, Seibel R, Erbel R . Comparison of electron beam computed tomography with intracoronary ultrasound and coronary angiography for detection of coronary atherosclerosis. J Am Coll Cardiol 1997; 30: 57–64.
Nallamothu BK, Saint S, Bielak LF, Sonnad SS, Peyser PA, Rubenfire M, Fendrick AM . Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis. Arch Intern Med 2001; 161: 833–838.
Rumberger JA, Brundage BH, Rader DJ, Kondos G . Electron beam computed tomographic coronary calcium scanning: a review and guidelines for use in asymptomatic persons. Mayo Clin Proc 1999; 74: 243–252.
Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE . Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation 2006; 114: 1761–1791.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999; 130: 461–470.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte Jr M, Detrano R . Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827–832.
Prentice RL, Szatrowski TP, Fujikura T, Kato H, Mason MW, Hamilton HH . Leukocyte counts and coronary heart disease in a Japanese cohort. Am J Epidemiol 1982; 116: 496–509.
Sweetnam PM, Thomas HF, Yamell JG, Baker IA, Elwood PC . Total and differential leukocyte counts as predictors of ischemic heart disease: the Caerphilly and Speedwell studies. Am J Epidemiol 1997; 145: 416–421.
Madjid M, Awan I, Willerson JT, Casscells SW . Leukocyte count and coronary heart disease: implications for risk assessment. J Am Coll Cardiol 2004; 44: 1945–1956.
Erdogan O, Gul C, Altun A, Ozbay G . Increased immunoglobulin E response in acute coronary syndromes. Angiology 2003; 54: 73–79.
Waller PF . The immunology of eosinophils. N Engl J Med 1991; 324: 1110–1118.
Hällgren R, Venge P, Cullhed I, Olsson I . Blood eosinophils and eosinophil cationic protein after acute myocardial infarction or corticosteroid administration. Br J Haematol 1979; 42: 147–154.
Slungaard A, Vercellotti GM, Tran T, Gleich GJ, Key NS . Eosinophil cationic granule proteins impair thrombomodulin function. A potential mechanism for thromboembolism in hypereosinophilic heart disease. J Clin Invest 1993; 91: 1721–1730.
Mukai HY, Ninomiya H, Ohtani K, Nagasawa T, Abe T . Major basic protein binding to thrombomodulin potentially contributes to the thrombosis in patients with eosinophilia. Br J Haematol 1995; 90: 892–899.
Rohrbach MS, Wheatley CL, Slifman NR, Gleich GJ . Activation of platelets by eosinophil granule proteins. J Exp Med 1990; 172: 1271–1274.
Emanuele E, Falcone C, D′Angelo A, Minoretti P, Buzzi MP, Bertona M, Geroldi D . Association of plasma eotaxin levels with the presence and extent of angiographic coronary artery disease. Atherosclerosis 2006; 186: 140–145.
Niccoli G, Ferrante G, Cosentino N, Conte M, Belloni F, Marino M, Bacà M, Montone RA, Sabato V, Schiavino D, Patriarca G, Crea F . Eosinophil cationic protein: A new biomarker of coronary atherosclerosis. Atherosclerosis 2010; 211: 606–611.
Chihara J, Yamamoto T, Kurachi D, Kakazu T, Higashimoto I, Nakajima S . Possible release of eosinophil granule proteins in response to signaling from intercellular adhesion molecule-1 and its ligands. Int Arch Allergy Immunol 1995; 108: 52–54.
Tintut Y, Patel J, Territo M, Saini T, Parhami F, Demer LL . Monocyte/macrophage regulation of vascular calcification in vitro. Circulation 2002; 105: 650–655.
Libby P, Ridker PM, Maseri A . Inflammation and atherosclerosis. Circulation 2002; 105: 1135–1143.
Ridker PM . Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003; 107: 363–369.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tanaka, M., Fukui, M., Tomiyasu, Ki. et al. Eosinophil count is positively correlated with coronary artery calcification. Hypertens Res 35, 325–328 (2012). https://doi.org/10.1038/hr.2011.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.191
Keywords
This article is cited by
-
Do blood eosinophils strictly reflect airway inflammation in COPD? Comparison with asthmatic patients
Respiratory Research (2019)
-
Immune cell subset differentiation and tissue inflammation
Journal of Hematology & Oncology (2018)
-
White blood count and infarct size, myocardial salvage and clinical outcomes: the role of differentials
The International Journal of Cardiovascular Imaging (2014)
-
Meta-analyses of four eosinophil related gene variants in coronary heart disease
Journal of Thrombosis and Thrombolysis (2013)
-
Eosinophils: a new player in coronary atherosclerotic disease
Hypertension Research (2012)