Abstract
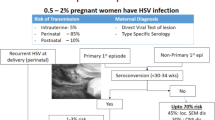
Herpes simplex viruses (HSV) are ubiquitous pathogens which can be transmitted vertically causing significant morbidity and mortality in neonates. Neonatal HSV infection is infrequent with an incidence ranging from 1 in 3500 to 1 in 20 000, depending on the population. Neonatal HSV infection is much more frequent in infants born to mothers experiencing a primary HSV infection with an incidence approaching 50%, while infants born to mothers experiencing recurrent HSV infection have an incidence of less than 3%.
Neonatal infections are clinically categorised according to the extent of the disease. They are: (i) skin, eye and mouth (SEM) infections; (ii) central nervous system infection (encephalitis) — neonatal encephalitis can include SEM infections; and (iii) disseminated infection involving several organs, including the liver, lung, skin and/or adrenals. The central nervous system may also be involved in disseminated infections.
Caesarean section, where the amniotic membranes are intact or have been ruptured for less than 4 hours, is recommended for those women who have clinical evidence of active herpes lesions on the cervix or vulva at the time of labour. This procedure significantly decreases the risk of transmission to the infant.
Diagnosis of neonatal infection requires a very high level of clinical awareness as only a minority of mothers will have a history of genital HSV infection even though they are infected. Careful physical examination and appropriate investigations of the infant should accurately identify the infection in the majority of cases. Treatment is recommended where diagnosis is confirmed or there is a high level of suspicion.
The current recommendation for treatment is aciclovir 20 mg/kg 3 times daily by intravenous infusion. Careful monitoring of hydration and renal function as well as meticulous supportive care of a very sick infant is also required. The newer anti-herpes agents, valaciclovir and famciclovir, offer no advantage over aciclovir and are not recommended for neonatal HSV infection.
Prognosis is dependent upon the extent of disease and the efficacy of treatment, with highest rates of morbidity and mortality in disseminated infections, followed by central nervous system infection and the least in SEM infection. However, SEM infection is associated with poor developmental outcome even in infants who do not have encephalitis. Studies to improve the outcome of SEM infection are in progress.
Neonatal HSV infections, although being relatively uncommon, are associated with significant morbidity and mortality if unrecognised and specific treatment is delayed. Diagnosis relies on a high level of clinical suspicion and appropriate investigation. With early therapy, the prognosis for this infection is considerably improved.


Similar content being viewed by others
References
Roizman B, Spears A. Herpes simplex viruses and their replication. In: Fields B, Knipe D, editors. Virology. New York: Raven Press, 1995: 1795–841
Whitley R, Lakeman F. Herpes simplex virus infections of the central nervous system: therapeutic and diagnostic considerations. Clin Inf Dis 1995; 20: 414–20
Whitley R, Arvin A. Herpes simplex virus infections. In: Klein JR, Klein J, editors. Infectious diseases of the fetus and newborn infant. Philadelphia (PA): Saunders, 1995: 354–76
Prober C, Sullender W, Yasukawa L, et al. Low risk of herpes simplex virus in neonates exposed to the virus at the time of vaginal delivery to mothers with recurrent genital herpes simplex virus infections. N Engl J Med 1987; 316: 240–4
Whitley R, Arvin, A, Prober C, et al. A controlled trial comparing vidarabine with acyclovir in neonatal herpes simplex virus infection. Infectious Diseases Collaborative Antiviral Study Group. N Engl J Med 1991; 324: 444–9
Whitley R, Hutto C. Neonatal herpes simplex virus infections. Pediatr Rev 1985; 7: 119–26
Sakaoka H, Saheki Y, Uzuki K, et al. Two outbreaks of herpes simplex virus type 1 nosocomial infection among newborns. J Clin Microbiol 1986; 24: 36–40
Dyke RV, Spector S. Transmission of herpes simplex virus type 1 to a newborn infant during endotracheal suctioning for meconium aspiration. Pediatr Infect Dis 1984; 3: 153–6
Brown Z, Benedetti J, Ashley R, et al. Neonatal herpes simplex virus infection in relation to asymptomatic maternal infection at the time of labor. N Engl J Med 1991; 324: 1247–52
Corey L, Adams H, Brown Z, et al. Genital herpes simplex virus infections: cinical manifestations, course and complications. Ann Intern Med 1983; 98: 958–72
Overall J. Empiric therapy with acyclovir for suspected neonatal herpes simplex infections. Pediatr Infect Dis J 1989; 8: 808–9
Overall J. Herpes simplex virus infections of the fetus and newborn. Pediatr Ann 1995; 23: 131–6
Whitley R, Yeager A, Kartus P, et al. Neonatal herpes simplex virus infection: follow-up evaluation of vidarabine therapy. Pediatrics 1983; 72: 778–85
Whitley R, Arvin A, Prober C, et al. Predictors of morbidity and mortality in neonates with herpes simplex infection. N Engl J Med 1991; 324: 450–4
Hutto C, Arvin A, Jacobs R, et al. Intrauterine herpes simplex virus infections. J Pediatr 1987; 110: 97–101
Frenkel L, Brown Z, Bryson Y, et al. Pharmacokinetics of acyclovir in the term human pregnancy and neonate. Am J Obstet Gynecol 1991; 164: 569–76
Whitley R, Gnann J. Acyclovir: a decade later. N Engl J Med 1992; 327: 782–9
Whitley R, Nahmias A, Visintine A. et al. The natural history of herpes simplex virus infections in the mother and neonate. Pediatrics 1980; 66: 489–94
Lakeman F, Whitley R, Diagnosis of herpes simplex encephalitis: application of polymerase chain reaction to cerebrospinal fluid from brain-biopsied patients and correlation with disease. National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. J Infect Dis 1995; 171: 857–63
Lau R, Emery M, Galinsky R, et al. Unexpected accumulation of acyclovir in breast milk. Obstet Gynecol 1987; 69: 468–71
Reiff-Eldridge R, Heffner CR, Ephross SA, et al. Monitoring pregnancy outcomes after prenatal drug exposure through prospective registries: a pharmaceutical company commitment. Am J Obstet Gynecol 2000; 182: 159–63
Coen DM. The implications of resistance to antiviral drugs for herpes virus drug targets and drug therapy. Antiviral Res 1991; 15: 287–300
Draby G, Larder BA. The clinical significance of antiviral drug resistance. Res Virol 1992; 143: 116–20
Gateley A, Gander RM, Johnson PL, et al. Herpes simplex virus type 2 meningoencephalitis resistant to acyclovir in a patient with AIDS. J Infect Dis 1990; 161: 711–5
Kimberlin D, Jacobs R, Powell D, et al. The safety and efficacy of high dose acyclovir in neonatal herpes simplex virus (HSV) infections [abstract]. Pediatr Res 1999; 45 (Pt 2): 165A
Prober C, Hensleigh P, Boucher F, et al. Use of routine viral cultures at delivery to identify neonates exposed to herpes simplex virus. N Engl J Med 1988; 318: 887–91
Kohl S. A hypothesis on the pathophysiology of neonatal herpes simplex virus encephalitis: clinical recurrence after asymptomatic primary infection. Pediatr Infect Dis J 1990; 9: 307–8
Kimberlin D, Powell D, Graber W, et al. Administration of oral acyclovir suppressive therapy after neonatal herpes simplex virus disease limited to the skin, eyes and mouth: results of a phase I/II trial. Pediatr Infect Dis J 1996; 15: 247–54
Arvin A, Hensleigh P, Prober C, et al. Failure of antepartum maternal cultures to predict the infant’s risk of exposure to herpes simplex virus at delivery. N Engl J Med 1986; 315: 796–800
Brocklehurst P, Kinghorn G, Carney O, et al. A randomised placebo controlled trial of suppressive aciclovir in late pregnancy in women with recurrent genital herpes infection. Br J Obstet Gynaecol 1998; 105: 275–280
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kesson, A.M. Management of Neonatal Herpes Simplex Virus Infection. Paediatr Drugs 3, 81–90 (2001). https://doi.org/10.2165/00128072-200103020-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00128072-200103020-00001